
NHS England will work alongside three major drugs companies in a bid to become the world’s first country to eliminate hepatitis C by 2025.
The healthcare body hopes the availability of new medicine created by US pharmaceutical firms Gilead Sciences, Merck & Co and AbbVie will help diagnose and treat those who may be unaware they are infected with the deadly virus.
About 113,000 people are chronically infected with hepatitis C – also known as HCV – in England, according to a 2019 report by government body Public Health England.
The Hepatitis C in England 2019 study also states that most people infected with the condition originate from marginalised and under-served groups in society.
NHS England’s chief executive Simon Stevens said: “It’s not often that the opportunity arises to completely eradicate a disease, but now the NHS is taking practical action to achieve exactly that.
“The NHS’s sophisticated and unashamedly rigorous negotiation on behalf of both patients and taxpayers means we’ve now been able to strike affordable deals with our life sciences partners to save many more lives and meaningfully cut health inequalities.”
What is hepatitis C?
Hepatitis refers to an inflammation of the liver cells and significant damage to the liver, mostly caused by a virus known as viral hepatitis, which consists of five different types.
According to the World Health Organization (WHO), the five types are identified as types A, B, C, D and E, all of which can cause deaths and illnesses – as well as the potential threat for outbreaks and epidemic spread of the disease, particularly with types B and C.
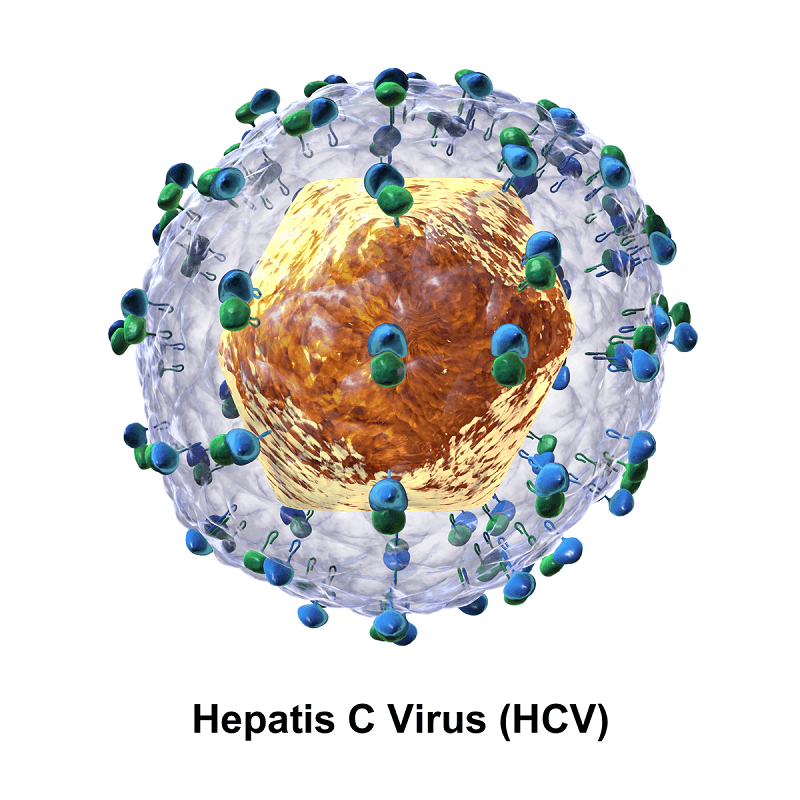
HCV is the most common type of viral hepatitis caused by a blood-borne virus that attacks the liver and is easily spread by sharing blood products such as needles, which could be used during medical procedures.
As there is no vaccine for HCV, most people are offered 12 weeks of tablets with few side effects and has a recovery rate of between of 90% and 95%, which more than 30,000 people have benefited from in England.
The new Public Health England data shows that deaths from serious HVC-related liver disease fell from 380 to 319 between 2015 and 2017, as a result of new curative treatments.
However, while England has exceeded WHO’s target to reduce HVC related mortality by 10% by 2020, challenges still exist to eliminate the disease.
How will the NHS ENgland partnership achieve hepatitis elimination?
The three-year partnership with Gilead Sciences, Merck & Co and AbbVie will work to eliminate HCV as a major public health issue in England, five years earlier than the WHO goal of 2030.
Five new HCV drugs will be available at “the best price”, NHS England claimed.
Programmes with local health services, councils and voluntary groups will be launched to find patients and provide testing and treatment, including the homeless and those living with mentally illnesses.
James Mather, a senior pharma analyst at market intelligence firm GlobalData, said: “The approach planned by NHS England, along access to direct-acting antivirals (DAAs) from the partnered companies, is to target currently undiagnosed and under-treated populations, including the homeless and mentally ill.
“This targeted approach will lead to a rapid increase in diagnosis rate among these populations, coupled with the high cure rate of DAAs, will cause the hepatitis C prevalence to drop significantly to approximately 2,750 in the UK, by 2026.”
The NHS has said the contract will be worth almost £1bn and is the latest initiative in a series of “smart deals”.
“The procurement approach of NHS England has allowed it to negotiate low prices with Gilead, Merck and AbbVie for five hepatitis C therapies,” added Mr Marther.
“As we approach the WHO’s target for the elimination of hepatitis C by 2030, GlobalData expects that more deals will be struck between these three companies and public health bodies globally.
“Gilead has already secured a first of its kind subscription based deal to supply Louisiana’s Department of Health, and other US health departments are now seeking similar partnerships.”






