Throughout much of 2020, 3D printing — or additive manufacturing (AM) — has been used in a variety of ways to ease the burden of Covid-19 on healthcare systems and patients. Dr Gautam Gupta, vice president and general manager of medical devices at 3D Systems, discusses the growing number of applications it has in the world of surgery.
The speed at which healthcare innovation is occurring – from the way surgeries are performed, to the development of new therapies – is accelerating.
Healthcare providers have become increasingly reliant on innovative technologies to improve patient care.
With the advent of the global pandemic, timely healthcare delivery was put to the test, and additive manufacturing demonstrated its power as an enabling solution.
As Covid-19 cases increased, healthcare workers needed increased volumes of PPE (personal protective equipment) to treat patients.
Additionally, the need for ventilators was growing exponentially and production lines came to a halt as raw materials were unavailable.

Critical shortages eased by 3D printing
The pandemic disrupted supply chains and AM was highlighted for its ability to rapidly produce the necessary items.
When it came to manufacturing of nasopharyngeal swabs, for example, AM enabled rapid innovation via multiple design and material iterations to launch a product that could be mass-produced cost-effectively.
As a result, several contract manufacturers were able to adapt their shop floors overnight to produce these swabs.
Similarly, multiple hospitals brought the technology on-site to produce swabs – achieving greater control of their supply chain.
Yet with all the advances, findings by the World Health Organisation (WHO) suggest that globally, surgery still results in high rates of illness, disease, and death.
Unsafe surgical care procedures cause complications in up to 25% of patients.
Almost seven million surgical patients suffer significant complications, one million of whom die during or immediately following surgery.
Long before the pandemic, additive manufacturing was recognised for its ability to enable the creation of personalised surgical plans and tools, thus helping improve patient outcomes.
Personalising surgery with 3D printing
US-based firm 3D Systems introduced the industry to Virtual Surgical Planning (VSP).
VSP combines expertise in medical imaging, surgical simulation, and 3D printing to enable personalised surgery – allowing surgeons to perform the surgery digitally before entering the operating room.
Following an online planning session, patient-specific models, guides, and templates are designed and 3D printed for use within the sterile field.
If these capabilities could be located within the healthcare institution – at the point of care – the planning and delivery time could be condensed.
This is already occurring at some of the world’s elite hospitals where clinicians can create customised solutions for patient care using AM solutions available to them on campus.
Benefits of patient-specific models
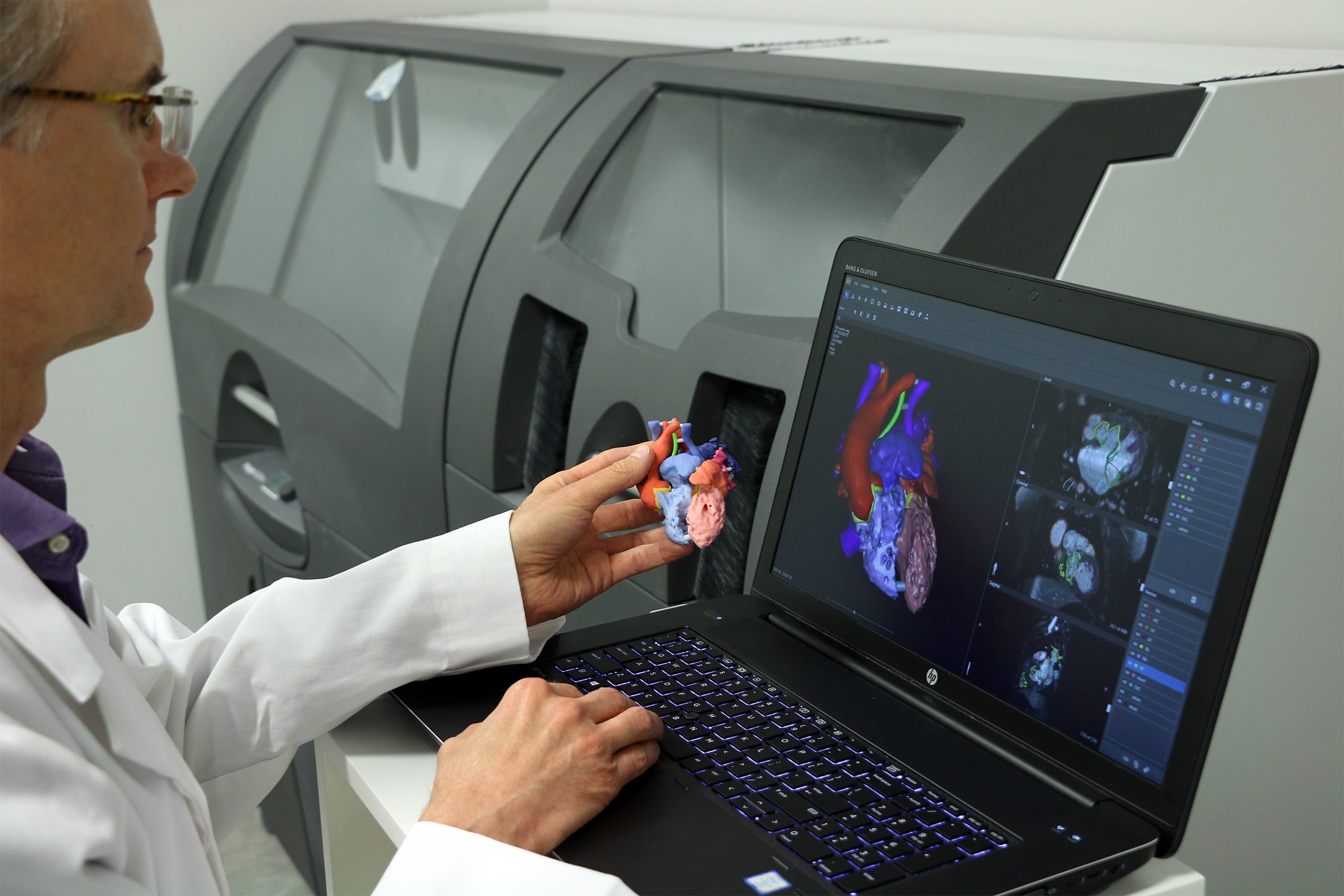
To create patient-specific models, the clinician must first begin with scans of the patient anatomy.
FDA-cleared software is available that relies on unique automatic segmentation tools driven by deep learning enabling medical practitioners to quickly create accurate, digital 3D anatomic models from medical imaging data.
The models, in combination with the pre-surgical plan, allow clinicians to design patient-specific tools and guides for use during the procedure.
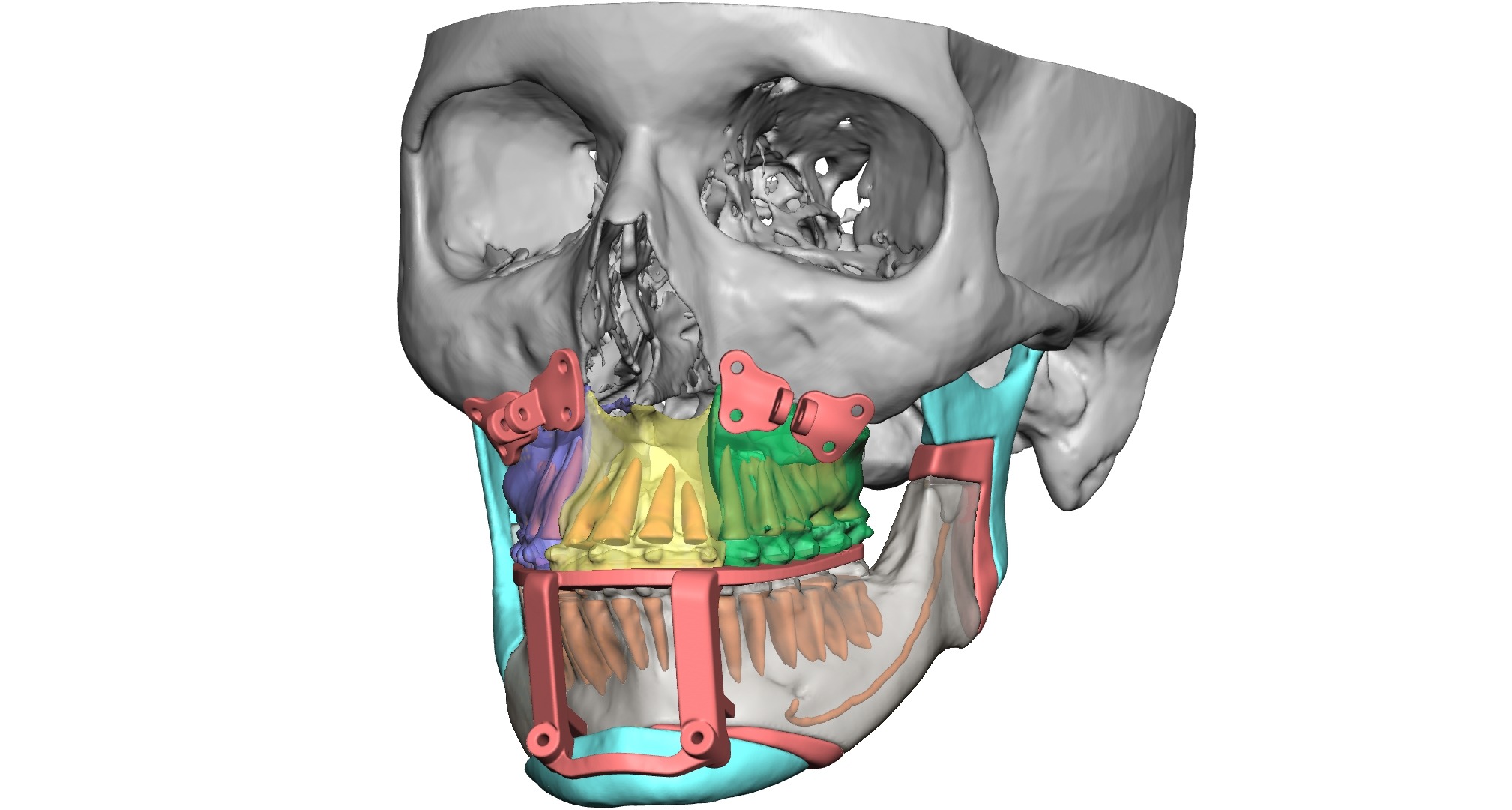
This is accomplished using 3D design software that includes advanced tools for working with complex, organic shapes like patient anatomy.
This software – in combination with a haptic device – facilitates user-friendly interaction with the modelling shape to create precise devices.
Having a 3D printer at the point of care allows efficient production of models and tools for use within the sterile field.
Improving patient satisfaction
Complex surgical procedures are stressful for patients and their families due, in part, to not having a good understanding of what will occur in the operating room.
Employing point of care solutions can arm surgeons with the tools needed to improve pre-surgical planning.
Moreover, surgeons can use the 3D models as visual tools to educate patients and their family through the procedure.
This provides a level of reassurance that the plan has been thoroughly thought through to achieve the desired outcome.
In clinical applications where VSP is used today, the solutions have been shown to improve surgical accuracy and outcomes, saving time in the operating room – which benefits both the surgeon and the patient.
Designing the optimal surgical plan also includes conducting the procedure in a way that is the least invasive, helping to reduce the length of stay, and ultimately overall healthcare costs.
The future of patient-centric innovation
AM continues to accelerate healthcare innovation, yet at the point of care, the technology is still in its infancy.
As the technology becomes more user-friendly for medical professionals, a larger number of hospitals will be able to implement end-to-end solutions for personalised care.
The opportunity to have this capability on-site will go beyond improving accuracy and efficiency of surgical procedures.
Clinicians will be able to make strides in their own innovation, enhancing R&D efforts.
They will be able to enhance the training of staff through the use of 3D models and VR (virtual reality).
Most importantly, AM has tremendous potential to shape the future of healthcare by disrupting existing models to improve the quality of care.






