Researchers have established demand for their rapid traumatic brain injury detection technique across eight countries by working with non-departmental government accelerator Innovate UK

The published research behind the technique revealed the importance of rapid detection for brain injury (Credit: PixaBay)
A method for traumatic brain injury (TBI) detection at the point of care has been developed by scientists in the UK, and they’re now developing a device to apply it in emergency situations.
Using chemical biomarkers released by the brain immediately after a head injury occurs, the researchers were able to pinpoint when patients needed urgent medical attention – a breakthrough that could save time in delivering vital treatment and avoid patients undergoing unnecessary testing.
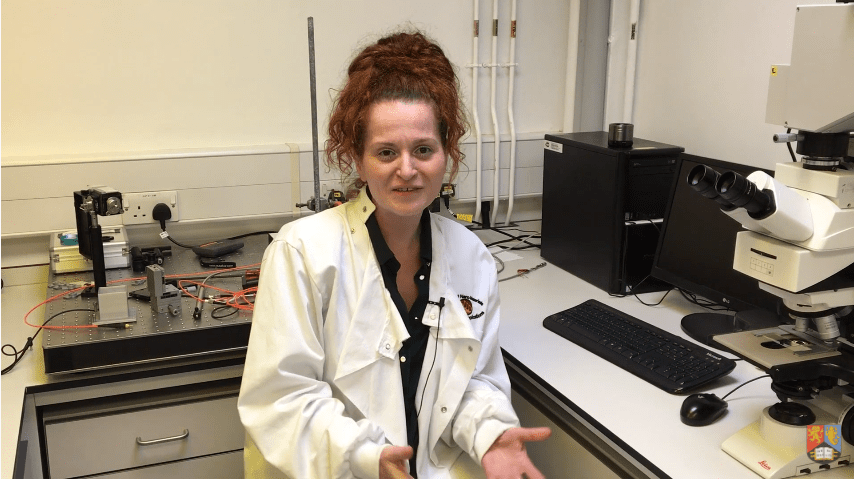
The technique was developed by a multi-disciplinary team of researchers in the group of Advanced Nanomaterials, Structures and Applications (ANMSA) at the University of Birmingham, led by Dr Pola Goldberg Oppenheimer.
“This is a relatively straightforward and quick technique that offers a low cost, but highly accurate way of assessing traumatic brain injury, which up until now has not been possible,” said Dr Oppenheimer.
“The current tools we use to diagnose TBI are really quite old fashioned, and rely on the subjective judgement of the paramedic or the emergency doctors.
“There’s an urgent need for new technology in this area to enable us to offer the right treatment for the patient, and also to avoid expensive and time-consuming tests for patients where there is no TBI.”
The researchers drew attention to a study from brain injury charity Headway, which found roughly 1 million people each year visit A&E following a head injury, in order to show the scale of the problem they’re seeking to solve.
Following a proof-of-concept study, the ANMSA group completed Innovate UK’s commercialisation programme, iCURE, to identify commercialisation routes for the technique – a process that identified potential partners across eight countries.
According to the university, additional funding from the Royal Academy of Engineering led to a market analysis including paramedics, neurosurgeons and sports therapists – all of which also confirmed a strong demand for the technology.
How do researchers use biomarkers to detect traumatic brain injury?
Current methods of assessing TBI frequently rely on the Glasgow Coma Scale, in which clinicians make a subjective judgement based on the patient’s ability to open their eyes, their verbal responses and their ability to move in response to an instruction.
The method discovered by the ANMSA researchers works using a spectroscopic technique called surface enhanced Raman scattering, in which a beam of light is fired at the biomarker – a naturally occurring molecule, gene, or characteristic that indicates some form of disease state.
The biomarker, taken from a pin prick blood sample, is prepared by being inserted into a special optofluidic chip, where the blood plasma is separated and flows over a highly specialised surface.
The light causes the biomarker to vibrate or rotate and this movement can be measured, giving an accurate indication of the level of injury that has occurred.
To produce the level of accuracy required, the test needs to be extremely sensitive, the key to which is in the way the biomarkers interact with the surface.
The team developed a low-cost platform, made from polymer and covered with a thin film of gold.
This structure is then subjected to a strong electric field, which redistributes the film into a distinctive pattern, optimised to resonate in exactly the right way with the light beam.
Research highlighted need for rapid brain injury detection device
Research demonstrating the technique was published in the journal Nature Biomedical Engineering.
In the study, 48 patients were assessed using the engineered device, with 139 samples taken from patients with TBI and 82 from a control group.
The study showed that in the TBI group, the levels of the biomarker were around five times higher than in samples taken from the control group.
The team also found the levels tailed off rapidly around one hour after the injury occurred, further highlighting the need for rapid detection.
According to the researchers, the next stage will be to miniaturise the device technology used to analyse the samples, so that it could be easily stored on board an ambulance for use by paramedics, used at sporting events where head injuries can be hard to detect, at local GP services or in hospitals where it could be used over time to monitor patients to see how the head injury is progressing.
The team said it is currently working towards optimising and trailing a prototype technology on a larger patient cohort for these applications.
