
Management of heart failure could soon be easier for cardiologists after an Israeli start-up developed technology that can be implanted inside the body to remove excess fluid around-the-clock.
Paragate Medical will soon begin large-scale human clinical trials on its Implantable Peritoneal Ultrafiltration Device (IPUD), which is aimed at congestive heart failure patients and remains active 24 hours a day.
Fluid congestion remains a primary issue for patients with chronic heart failure and is a major cause of deaths.
According to US Emory Healthcare, nearly five million Americans live with congestive heart failure, and approximately 550,000 new cases are diagnosed in the US each year.
Paragate co-founder and CEO Nitai Hanani told Compelo: “Congestion is the reason for nine out of ten heart failure hospitalisations.
“Although patients are admitted for acute episodes, what they actually have is a chronic condition that is treated acutely and, therefore, not very successfully.
“The biggest advantage the IPUD offers is the reduced burden associated with repeated hospitalisations for all stakeholders.
“Patients benefit from an improved quality of life.”
History of Paragate Medical
Based in Nazareth, Paragate Medical was founded in 2016 by biomedical engineer Mr Hanani and cardiologist Dr Yair Feld, who is the company’s medical director.
Dr Feld was inspired with the idea of a “parallel gate”, a mechanical bypass that already exists for the kidney, after encountering a patient who suffered from extreme conditions of congestion and urine production.
He observed the bed sheets were constantly soaked due to the leakage of oedema fluid – abnormal accumulation of fluid located beneath the skin and cavities of the body.
The fluid would seep through the old and bruised skin, exiting the body along with some toxins.
After observing this, Dr Feld decided to develop his own implantable device for the continuous relief of congestive heart failure patients’ clinical symptoms.
What is the Implantable Peritoneal Ultrafiltration Device for management of heart failure?

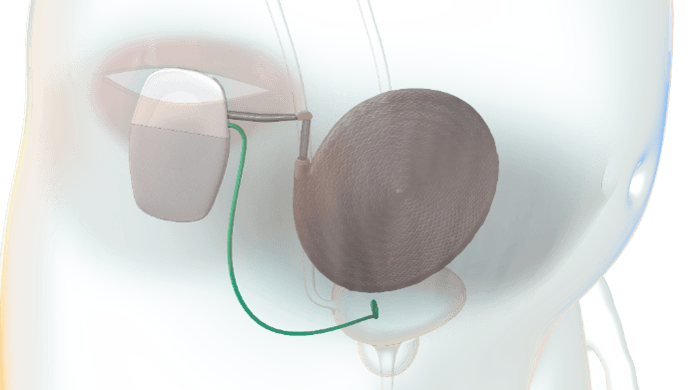
Paragate’s IPUD claims to be the “first ever implantable device to actively and continuously treat fluid overload.”
Peritoneal refers to the serous membrane, which forms the lining of the abdominal cavity and secretes a fluid that fills body cavities.
The device requires no external ports, and provides a minimally invasive system that removes excess extracellular fluid – such as glucose and salts – from the body.
Mr Hanani said: “Our approach is unique by offering a chronic solution for this chronic condition.
“Imagine a fully implantable device that can act 24/7 non-aggressively, clearing systemic excess fluid into the bladder, in a controlled and configurable manner – keeping the patient balanced at home.
“Unlike conventional treatments and other pipeline solutions, the IPUD has no access to the blood.
“The device doesn’t rely on dialysis [the process of removing excess water, solutes and toxins from the blood], so no dialysate should be injected into the peritoneal cavity.
“The device works on a direct mechanical principle that is not dependent on the intrinsic kidney’s function.”
How does the IPUD help the management of heart failure?
Paragate’s IPUD will be used by a cardiologist after a patient fails to respond to conventional oral diuretics – better known as “water pills” – which rid the body of unneeded water and salt as a common treatment for the management of heart failure.
Mr Hanani said: “The device can be implanted in patients if they’re eligible for surgery, by either electively or once stabilised after acute heart failure.
“The laparoscopic-compatible device allows a minimally-invasive, single-port, simple implantation.
“The cardiologist can begin the therapy treatment tailored to the patient’s needs.
“The system continuously collects therapy and physiological data that are transmitted to the physician’s management platform.
“We expect it to be just like ventricular assist devices (VAD), where patients arrive on a quarterly basis for an office visit to manage the therapy in accordance to their clinical condition.
“In the future, the system may be able to utilise the remotely sensed data to operate in a fully autonomous mode.”
How the IPUD can surpass current treatment methods for congestive heart failures
The machine’s ability to function outside hospital could have a positive financial impact, believe the Paragate founders.
They estimate healthcare budgets to reach up to to $100,000 (£77,730) per congestive heart failure patient, but this could be significantly reduced.
Mr Hanani, who has so far conducted tested the technology on a small number of patients, said: “Care providers can shift the weight of treatment towards a home setting, reduce the amount of complications due to aggressive treatments and reduce the penalties associated with frequent admissions.”
He believes there will also be a decrease in “frequent flyer” patients – who repeatedly show up in an emergency room for medical care.
“Those patients could have further complications such as hemodynamic shocks, worsening of renal function and infections, not to mention general hospital-acquired infections – so this will hopefully happen less,” he added.



