The new blood test detects DNA fragments released by damaged cells, which helps in determining disease severity in pulmonary arterial hypertension (PAH) patients
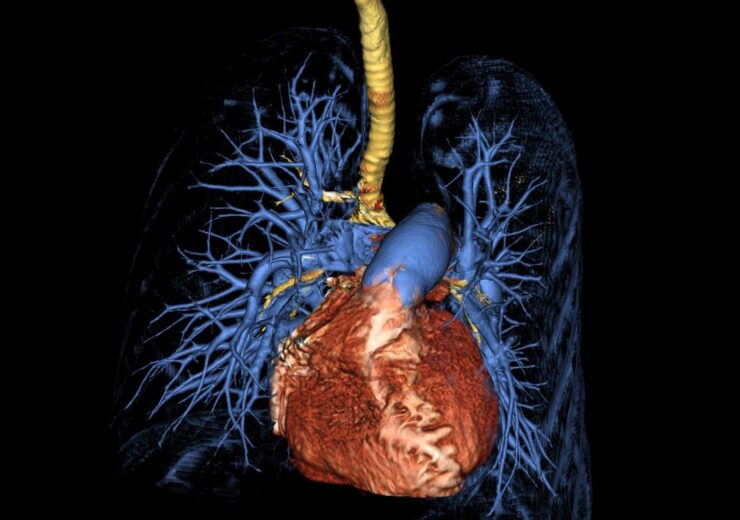
Computed tomography 3D surface rendering of the lungs and heart from a patient with pulmonary arterial hypertension. (Credit: NIH)
A study funded by the National Institutes of Health (NIH) in the US has shown that a new blood test can be used to determine disease severity in patients with pulmonary arterial hypertension (PAH) and assess survivability.
PAH is a rare condition that causes high blood pressure in the lungs triggering difficulty in breathing, chest pain, and fatigue. It narrows and blocks the small pulmonary arteries of the lungs and may result in death from heart failure.
NIH researchers have found that the new blood test quantifies DNA fragments released by damaged cells and these fragments, known as cell-free DNA, are higher in the blood of PAH patients. The presence of the damaged cells also increases with the severity of the condition.
According to the early clinical investigations, the test outperformed more traditional diagnostics, some of which utilise intrusive instruments.
This blood test for PAH patients may enable medical professionals to act more quickly to stop or slow the disease’s progression and save lives.
NIH said that the current methods for assessing the severity of PAH rely on known risk prediction scores based on clinical symptoms and on the intrusive use of a catheter to detect lung pressure.
Echocardiography, or heart imaging, is occasionally employed to measure the pressures in the heart to determine the pressures in the lungs indirectly. However, these tests lack sensitivity and reliability.
In the study, the research team examined cell-free DNA from blood samples collected from 209 adult patients, mostly women, who had been diagnosed with PAH at two major US medical facilities.
The results were compared with cell-free DNA obtained from 48 healthy volunteers without PAH who served as a control group and was assessed at the NIH Clinical Center.
They discovered that the amounts of cell-free DNA were raised in patients with PAH and rose proportionately to the disease’s severity.
According to NIH researchers, patients with the highest levels of cell-free DNA had 3.8 times higher risk of dying or needing a lung transplant than patients with the lowest levels.
Additional examinations of cell-free DNA samples revealed that PAH had an impact on a variety of tissue types, including the heart, blood vessels, adipose tissue, and inflammatory cells flowing through the circulation.
NIH entities- the National Heart, Lung, and Blood Institute (NHLBI) and the NIH Clinical Center, funded the study.
