Medical devices like scalpels have been around for thousands of years, but it is only with the advancement of 3D printing in the 1980s that manufacturers were able to adapt surgical instruments to make them more precise. It’s this precision that sets 3D printing apart from other medical advancements. The technology has allowed doctors and surgeons to provide individualised medical care to patients, whether that’s printing prosthetics, medical aids, tools, equipment, implants or plastic anatomical models known as ‘medical phantoms’.
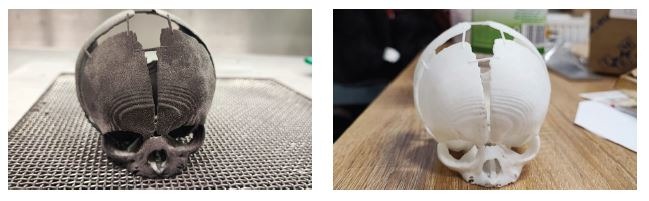
These medical phantoms hit the headlines over the last two years after surgeons, in several different cases, successfully separated conjoined twins thanks to 3D-printed models of patients’ brains, skulls and blood vessels, allowing them a controlled environment on which to practice, thereby reducing the risk of anatomical surprises.
In August this year, surgeons at University Children’s Hospital in Krakow, Poland, saved the life of a baby girl who was born without a fifth of her skull shortly after she’d been given only four days to live. Using 3D-printed skulls produced by Polish hardware R&D company Sygnis, one made from nylon and resins, the other from polymers, they were able to assess the extent of bone loss and plan the operation.
These incredible achievements wouldn’t have been possible without material scientists and engineers working alongside doctors to find the best materials for 3D printing. Material is often chosen based on three key criteria – biocompatibility, sterilisability and bio-usability – whether it has physical properties similar to the area of the body being replaced, such as its flexibility and strength.
The right material
Plastics such as acrylonitrile butadiene styrene (ABS) or nylon are the materials of choice for 3D-printed prosthetics and medical models, because of their malleability and lightweight properties. These include polylactic acid (PLA), a thermoplastic polyester which is commonly used to create biodegradable limb sockets, screws and pins, but can also be used for bone scaffolds and drug delivery systems. Two popular thermoplastic polymers are Polyetheretherketone (PEEK) and Polyetherketoneketone (PEKK) and are commonly used for 3D-printed implants for bone and cartilage replacement because of their strength and biocompatibility.
Acrylic or polymethyl methacrylate (PMMA), otherwise known as ‘bone cement’ is used to fill in the gaps between implants and bones, as well as to make surgical tools. It makes good dentures and fillings too as it’s easy to dye to match the colour and size of a patient’s teeth. In the same way, bio-ceramics such as hydroxyapatite (HA) and tricalcium phosphate (TCP) are used for dental implants like crowns because of their similarity to teeth and bone.
Although ‘skin friendly’ silicone is used for implants, 3D printing on this particular material is still in its early stages. Challenges include the time it takes to print and its high viscosity, which makes it difficult to print to the standard needed. However, engineers are busy developing and perfecting 3D printers for silicone to bring more medical devices created using the material to market.
Tough enough
One material that stands out for many surgeons and researchers using 3D technology for implants is titanium. Professor Mika Salmi is research director for the Aalto Digital Design Laboratory at Aalto University and has seen a huge increase in personalised treatment through 3D printing using titanium in recent years, especially in implants. He works in collaboration with surgeons at Finland’s Helsinki University Hospital on 3D printing personalised medical devices, for example, for patients with maxillofacial injuries caused by accidents, and tumours where bone has been damaged or needs to be removed.
“3D printing cannot yet make the perfect material and so you need to select something that is good enough, and quite often that is titanium,” he explains. “We obviously work very closely with doctors who use medical imaging and from the layer images, we can calculate what the patient’s bone would look like and use that to create our 3D model.”
Polymers come in handy in Salmi’s lab too though, as his team create pre-operative models made of plastic so that surgeons can better plan operations. “A volumetric titanium net structure implant can then be 3D printed, which allows tissues to grow through and attach to other surrounding tissue,” he says. “Implants are attached to bone with titanium screws.”
Titanium is also used to 3D print joint replacements and dental implants, while another type of metal, cobalt chrome, is widely used for replacement joints, like hips, shoulders and knees. As well as being used for surgical tools, stainless steel can also be used to print temporary implants.
The future is here
The world of 3D printing in medicine sometimes sounds like something straight out of science fiction. Especially materials such as Polyethylene glycol (PEG), a polyether compound derived from petroleum, that is helping scientists push the boundaries of regenerative medicine and 3D tissue printing in a newer class of additive manufacturing known as ‘bioprinting’. This method of 3D printing involves a mixture of living cells and biomaterials, or bioinks, used to create organ-like structures that allow patients’ cells to multiply and is part of the growing field of regenerative medicine. PEG is one of the materials used because it mimics our cells’ physical and biochemical characteristics.
“We have printed bone, cartilage, and muscle tissue that, when implanted in experimental models, developed a system of nerves and blood vessels.”
Professor Anthony Atala
Professor Anthony Atala is director of Wake Forest Institute for Regenerative Medicine (WFIRM) in the USA, and his team developed the Integrated Tissue and Organ Printing (ITOP) System after starting out engineering tissues in the lab by hand. He was inspired to research the possibility of providing replacement tissues and organs after working as a paediatric urologic surgeon. “It’s devastating to both the patient and doctor when a patient needs replacement tissue for reconstruction and there is not a good option,” he says. “There is generally a Plan B, such as taking tissue from other organs, but it is almost never ideal.”
Atala’s team have already implanted several tissues and organs in patients, such as skin, urethras, cartilage, bladders, muscle and vaginal organs – all created by hand. Their next goal is to be able to do the same using bioprinting. “This will allow us to automate the process and scale up the technology so it can be applied to many more patients,” he says.
“We are working on developing replacement organs and tissues, as well as healing cell therapies, for more than 40 different areas of the body.” Projects range from blood vessels and kidneys to cell therapies for lung disease and haemophilia. “We are pursuing multiple strategies, including 3D printing, to move our projects forward to meet our ultimate goal – making patients better,” he adds. In fact, in 2021, the WFIRM fielded two teams in NASA’s Vascular Tissue Challenge and took first and second place.
In terms of the best biomaterials for 3D printing, Professor Atala says researchers have developed various biomaterial systems that improve cellular interactions by providing appropriate environmental cues. These biomaterial systems consist of drug/ protein delivery systems, nano and micro-scale topographical features and hybrid materials that can actively participate in functional tissue regeneration.
“Automated 3D bioprinting technology can manufacture complex, multi-cellular living tissue constructs that mimic the structure of native tissues,” he explains. “This can be accomplished by optimising the formulation of biomaterials to serve as the scaffolding for 3D bioprinting, and by providing the biological environment needed for the successful delivery of cells and biomaterials to discrete locations within the 3D structure.”
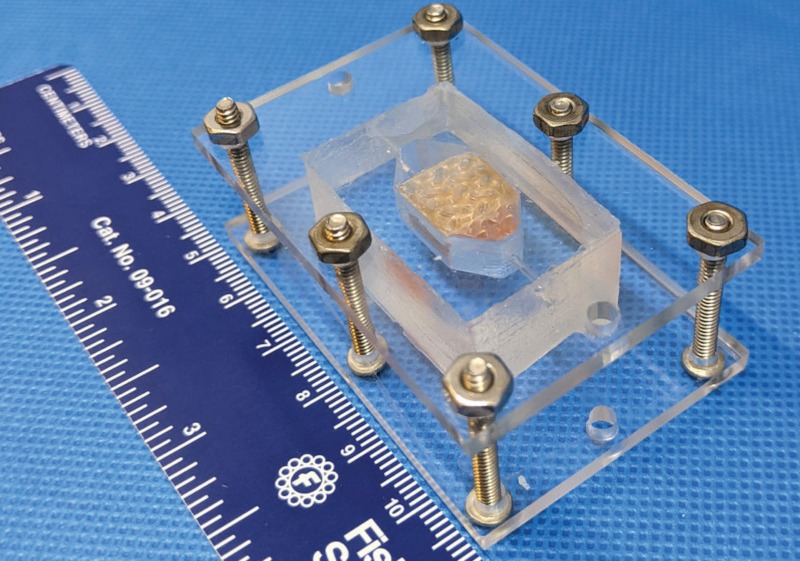
The first step in printing an organ or tissue structure for a patient is to expand the number of a patient’s cells in the laboratory to obtain the millions required to engineer replacement tissue. The printer has small nozzles to precisely deposit both biodegradable, plastic-like materials to form the tissue ‘shape’, and water-based gels that contain the cells. This water-based ‘ink’ – cells and the materials that form the shape – is optimised to promote cell health and growth. In addition, a lattice of micro-channels is printed throughout the structure to allow nutrients and oxygen from the body to diffuse into the structures. This last process keeps the cells alive while the tissues develop their own system of blood vessels.
“The system deposits both biodegradable, plastic-like materials to form the tissue ‘shape’ and water-based gels that contain the cells. In addition, a strong, temporary outer structure is formed,” said Atala. “We have printed bone, cartilage, and muscle tissue that, when implanted in experimental models, developed a system of nerves and blood vessels. We showed that these structures have the correct size, strength and function for use in humans, proving the feasibility of printing living tissue structures to replace injured or diseased tissue in patients.” Advancements in biomaterials science and the field of additive manufacturing are promising for multiple areas of medicine, and Atala is optimistic about what the future holds. He concludes: “We’re excited and encouraged by the ability of regenerative medicine to provide replacement tissue made from a patient’s own cells, and what that can mean for their recovery and long-term health.”






