For years, Messe Düsseldorf and the IVAM Microtechnology Network have been the joint hosts of the COMPAMED Innovation Forum. Each spring, with a different content focal point each year, there is a first look at the topics for the coming season of the internationally leading expert trade fair for suppliers of the medical technology industry, COMPAMED in Düsseldorf, which will be held this year from November 14 to 17, in parallel with the globally leading medical trade fair MEDICA. The 2022 COMPAMED Innovation Forum which is dedicated to “Innovative technology for neurological applications” was held virtually on June 2.
Presentations were focused on current products and their applications, some of which are still in the research and development phase, and some are already being put to use. In addition to implants, technical aids which are used to care for and assist people affected by neurological disorders play an important role. Addressing the participants of the forum, Christian Bigge, Senior Project Manager for COMPAMED at Messe Düsseldorf, was happy to pass on two messages: “We are planning for the event to happen in-person again and continue its success, enhanced by numerous digital services. Halls 8a and 8b, reserved for COMPAMED, will be completely booked out.”
Neurological and psychiatric disorders of the brain are not a rare phenomenon, but their frequency and their effects are still underestimated. These disorders affect the lives of many people and their families. According to an estimate by the WHO, a billion patients worldwide suffer from disorders of the central nervous system (CNS), such as depression, dementia, epilepsy, Parkinson’s, or the sequelae of a stroke. Treatment cannot solely consist of relying on medication alone. Innovative medical technology can also improve the quality of life of those affected. Unlike medication, which helps to regulate the chemical balance within the human body, neurological implants target the electrical neural pathways within the spinal cord and brain.
Advances in brain-computer interfaces
One important field of research for the Clinical Neurotechnology research section at the Charité university hospital in Berlin is the use of brain-computer or brain-machine interfaces (BCI/BMI) in combination with non-invasive brain stimulation methods, such as transcranial electric or magnetic stimulation (TES/TMS). Professor Surjo R. Soekadar, head of the Clinical Neurotechnology research section and head of the clinical department of Translation and Neurotechnology at Charité, reported on the current level of technological advancement. In 1999, Professor Nils Birbaumer had already proven that fully paralysed patients – without the ability to move or speak – could, by changing the electric activity in the brain, select individual letters on a screen and thus write a complete message. This approach has made enormous developmental progress over recent years, thanks to more powerful, faster computers and the increase in their memory capacities, as well as due to the use of artificial intelligence (AI) and machine learning.
The Professor Soekodar’s research section, for example, focuses on the examination of neuroplasticity in the context of BCI applications. Here, BCI systems are combined with other forms of neurological technology, e.g. non-invasive brain stimulation. Brain stimulation techniques have been used in a clinical environment for decades, in order to effect targeted changes in brain activity and thus promote neuroplasticity. The goal of combining both methods is to better understand and influence neuroplastic processes. This approach aims to yield new and effective therapeutic methods that offer individual treatment of disorders of the CNS with as few side effects as possible. Development over the recent years has proven that assistive and regenerative BCIs are effective clinical instruments for regaining movement. The combination of BCI and neurological modulation, or non-invasive brain stimulation, can in this case illuminate the causal relationship between brain waves, brain function and behaviour. The path forward is also clear: “Right now, quantum sensors are the most promising technology for advancing non-invasive BCI applications. However, there are still some challenges that need to be overcome, such as shielding and isolation,” says Soekadar, speaking as an expert at the COMPAMED Innovation Forum.
Brain Interchange platform technology
A platform technology for a brain interchange system for neurological therapy has been developed by CorTec, in cooperation with clinical partners. The focus is on components and devices that can be used by industry, scientists and clinical professionals alike. The BIC consists of all components necessary to achieve an electric connection between the neuronal system and external information technology. The exchange of information is performed to modulate the nervous system. The completely implantable system is calibrated for both recording and stimulation using 32 channels. It is intended for long-term monitoring and electrical stimulation of the central and the peripheral nervous system. The CorTec Brain Interchange receives electric signals from electrodes attached to the nervous system, and reinforces, digitalises and transmits these signals to a computing unit through an external unit. “Data processing takes place outside the body,” explains Dr Martin Schüttler, CTO of CorTec.
The company has announced further developmental progress. For example, preclinical trials and developmental milestones have recently been successfully concluded. During the next phases, the technology is to be fine-tuned and ultimately prepared for the first-in-human studies. The American bureau of regulations for medical products, the FDA, is currently looking into approving the brain interchange platform technology. The spectrum of possible applications is large, for example if a range of differently designed electrodes are used, and ranges from applications for Parkinson’s and epilepsy to treating chronic pain and movement disorders, which can result from major strokes, injuries to the spinal cord or progressive muscular dystrophy (ALS).
New mobility through brain waves and use of exoskeletons
The French company STATICE is a developer and contract manufacturer focusing on specific solutions in microtechnology and medical technology, including neurology. Injuries to the spinal cord above cervical vertebra C8 carry a large risk of the patient becoming tetraplegic and being unable to use their arms and hands. STATICE is aiming to restore mobility in such cases by combining the interpretation of brain waves with an exoskeleton. Towards the end of 2019, the medical journal “The Lancet” published results from the clinical study of a BCI project, in which French scientists from the CEA research centre and STATICE have proven the feasibility of control of an exoskeleton for tetraplegics. WIMAGINE neurological prosthetics play a crucial role. These are long-term implants placed on the dura mater, which record brain activity. The implantable matrix consists of 64 electrodes.
In September 2021, two patients with a C5 lesion of the spinal cord received such implants. To determine the stability of the signal during implantation, special metrics were used to evaluate the signal. The time-frequency charts obtained from task-focused instances of motor activation were also evaluated to monitor the long term activity of the electrodes. “It was possible to prove the long term functionality of the WIMAGINE implants for chronic implantation. With the help of up-to-date tools for signal analysis, we can record good stability of ECoG signals for each patient, which looks promising for clinical examination with epidural recordings.” says Benoit Studlé, CEO of STATICE, summarising the results. These are to be confirmed in further patients. The next step follows naturally: a wireless bypass of the damaged spinal cord for paraplegics. The impulses of motor intention transmitted by the brain are to be deciphered via WIMAGINE and then translated to impulses sent directly to the nerves that control the legs, for example.
Materials for implants and neurostimulation
Highly specialised devices and systems used in medical technology always need better and more highly functional materials. One supplier of such solutions is Sandvik. The company has a Medicine business unit, which focuses specifically on delivering materials for the cardiovascular, neurostimulation, remote monitoring and electronics fields. For example, Sandvik manufactures coated stainless steel fine wiring for the electrode arrangement, as well as cable and coil configuration for transmitting signals, and ball electrodes in hearing implants (cochlea). They are also working on is deep brain stimulation (DBS). This is a neurosurgical procedure which implants a neurostimulator to treat movement and neuropsychiatric disorders. “To stimulate nerves, we produce wires made of a platinum-iridium alloy and high quality conductive wires with a prolonged operating life,” explains Dr Cacie McDorman, Process Engineer Manager at Sandvik Materials Technology.
Order components the size of a grain of sand
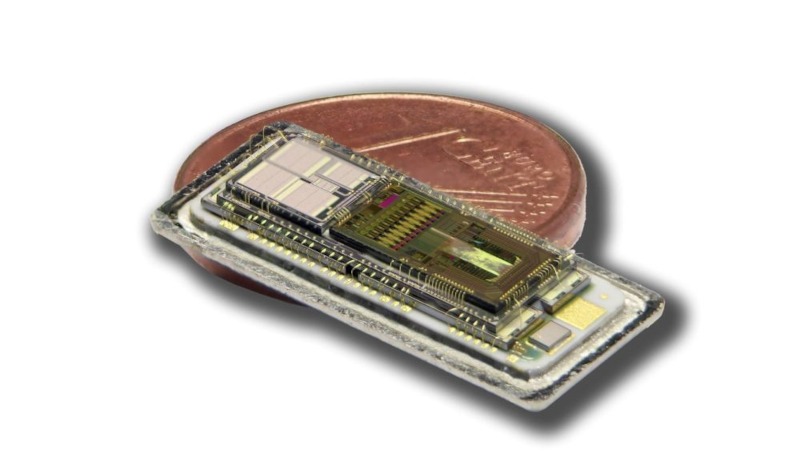
For 40 years, Valtronic has been a global full service licensed manufacturer of electronic products with a wealth of experience in ready-to-use production, microelectronic assemblies and miniaturisation. “Active implantable medical products are a challenge, from the design to manufacturing; just imagine the extreme miniaturisation, for example our DBS probes with a length of only 400 mm and a diameter of just 1.3 mm,” says Michael Fink, Consultant Business Development at Valtronic. Another example of this trend is the development of a thumb-sized device that sends programmable electric impulses to patients suffering from chronic pain, urinary incontinence and functional disorders of the limbs. The solution consists of minimised circuit complexity, and components reduced to the size of a grain of sand.
Mobile seizure detectors for recognising epilepsy
Epilepsy is a collective term for a group of functional disorders of the brain, which arise from the interaction of pathological excitation and lack of inhibition of excitation in the neuronal clusters of the CNS. Between 2 and 4 percent of all people suffer a single, isolated epileptic seizure. Between 0.5 and 1 percent develop manifest epilepsy, meaning that they have more than one seizure. Epilepsy is therefore one of the most common neurological disorders, affecting around 50 million people worldwide, with 800,000 in Germany alone. This considered, the Centre for Epileptology at the neurological clinic at the University Hospital of RWTH Aachen is researching seizure detection devices for affected patients. “The risks for epileptic patients are injuries, early death and damage to neurons, including the development of cognitive deficits over time,” says Prof Yvonne Weber, head of the epileptology section at the neurological clinic. Quite often, these risks lead to a lack of integration into social and working life, as well as to stigmatisation.
EEGs have been used to detect epileptic seizures up until this point. However, in recent years, the heart rate, which is increased in 60 to 70 percent of all cases, the variability of the heart rate, and also oxygen saturation and respiration levels have provided new measurands to detect epilepsy. In the Monikit (“monitoring kit”) project, the University Hospital of the RWTH Aachen, the Kleinwachau Centre for Epilepsy and the University Hospital of Tübingen University are developing a mobile seizure detection device for automatic detection and documentation of epileptic seizures that occur during daily activities. The comprehensive monikit system consists of a sensor array and an innovative algorithm. The sensor device is attached to the chest with adhesive electrodes or by belt, and picks up ECG and motion data. These data form the basis for the monikit algorithm and are transmitted to the patients’ mobile phone. “The small size of the sensor allows it to be worn underneath clothing. It has to be removed before taking a shower, though,” says Weber. The monikit algorithm recognises special patterns of both generalised and focal epileptic seizures from the ECG and motion data. This is made possible by machine learning methods, for example neuronal networks, which are trained on thousands of hours of patient data, which enables them to detect new digital biomarkers. The algorithm can differentiate between epileptic seizures and every day activities, like sports or stress. The monikit app automatically documents and evaluates any detected seizures. The app also sends messages in the event of a seizure, determines access rights, and collects statistical data about seizures.
Thus, doctors involved in treatment receive adequate and objective information about seizures during patients’ everyday activities for the first time. This makes optimum adjustment of the therapy possible. Once doctors have been legitimised and given access by the patient, they receive insight into seizure information through their internet browser, including evaluations of the course, type of seizure and other information – secured and encrypted according to standards. The project receives 1.86 m Euro in funding from the German Federal Ministry of Education and Research (BMBF), through the operating company Life Science Inkubator GmbH.
The market for neurostimulation is growing by more than 10 percent per year
There can be no doubt that the possibilities and possible applications for neurostimulation are increasing. According to findings by Allied Market Research, the global market volume for corresponding systems was estimated at around 4.4 billion US dollar in 2018, and is expected to expand to approximately 11.3 billion US dollar by 2026. This corresponds to annual growth of 12.5 percent. Factors such as an increase in lifestyle diseases like depression and chronic pain, the growing number of neurological disorders, and investments in neuroscience and neuroscientific development are regarded as the drivers behind the growth. Other factors are the rising demand for minimally invasive surgery, the introduction of technologically advanced products and the rising age of populations, which makes them more susceptible to neurological disorders like epilepsy, Parkinson’s, Alzheimer’s and chronic pain. According to statements by GlobeTech, neurological applications account for approximately 24 percent of the total market for active implantable medical devices (AIMD). The largest segment belongs to spinal cord stimulators (SCS) with a 35 percent share in the market, followed by inner and middle ear stimulators (cochlear and BAHA) with 21 percent, deep brain stimulators (DBS) with 14 percent and sacral nerve stimulators (SNS) with just under 10 percent.
COMPAMED: The most important industry meet-up is back, live in Düsseldorf
The technological progress in combating neurological disorders is quite remarkable, as proven by the COMPAMED Innovation Forum 2022. More advanced products from the innovation-driven supplier industry for medical technology will be presented at COMPAMED 2022, which will take place in mid-November again, in halls 8a and 8b of the Düsseldorf trade fair centre. The main themes will be: Micro and micro system technology, new materials, processing them and functional surfaces, additive manufacturing/3D printing, manufacturing and packaging as well as a wide range of services. These themes also provide the content framework for the two integrated expert forums: the COMPAMED HIGH-TECH FORUM by the IVAM Microtechnology Network and the COMPAMED SUPPLIERS FORUM by the Devicemed professional medium.
Information on COMPAMED 2022 (14 – 17 November) online: https://www.compamed-tradefair.com.
Author: Klaus Jopp, freelance technical writer for science and technology (Hamburg)






